Omicron surges: Indiana reports record 12,960 new COVID-19 cases
Indiana has again broken its previous record for new COVID-19 cases.
The Indiana Department of Health on Wednesday added an incredible 12,960 new COVID-19 cases to its official dashboard. All but 33 of these cases were confirmed on Tuesday.
Six days ago, the state surpassed the previous summit of 8,436 new cases recorded in early December 2020 and reported 12,020 new cases. The official sum for December 29 on the state dashboard now confirms 11,792 cases.
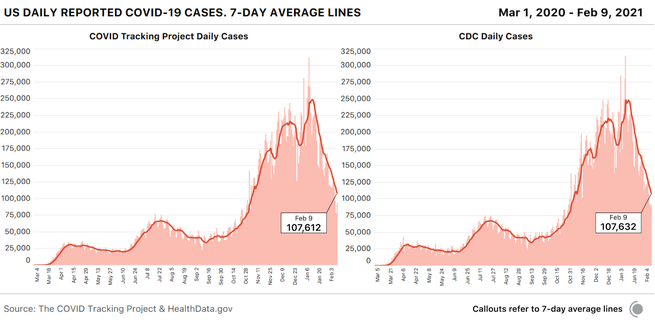
The seven-day average of new cases is now 9,251, higher than it has been at any other point of the pandemic to date.
COVID in Indiana: Indiana limits rapid testing due to lack
As of December 20, more than half of the cases found in the country were due to a version of omicron, the latest recurrence of the virus, which is much more contagious than its predecessors.
Although studies suggest that omicron may cause milder disease than the delta version that caused the recent rise in COVID-19, the number of hospitalizations in Indiana continues to increase. On Wednesday, Indiana reported 3,260 hospitalized for the virus, less than 200 less than the peak of 3,460 on Nov. 30, 2020.
State hospitals, however, are already struggling to control the influx of patients with COVID-19, along with a flood of those with other health problems. Just over 10% of beds in intensive care units are available, and emergency rooms are full of patients.
‘Stretched beyond prior belief’: Hospitals strive to cope with the latest rise in COVID-19
The level of positivity in Indiana also reached its highest point so far. Seven days ago, the last day with available data, the seven-day average positivity rate reached 22.5%. Prior to this last rise, the positivity rate in Indiana did not exceed 20%.
On Wednesday, health department officials announced earlier in the day that Chief State Health Commissioner Dr. Kris Box with a quick test positive for COVID-19. The box is fully vaccinated and had COVID-19 in the fall of 2020.
Although fully vaccinated and reinforced people can become infected with omicron, they are much less likely to develop a serious illness and need hospitalization, so health officials continue to strongly urge anyone who qualifies for vaccination.
Contact IndyStar rapporteur Shari Rudavsky at shari.rudavsky@indystar.com. Follow her on Facebook and Twitter: @srudavsky.
What pain medication can I take after the COVID-19 vaccine?

Centers for Disease Control says you can take over-the-counter pain medications such as ibuprofen (such as Advil), aspirin, antihistamines, or acetaminophen (such as Tylenol) if you have side effects after being vaccinated against Covid. This may interest you : David’s Sunday Evening Update. As with all medications, the CDC recommends that you talk to your doctor first.
Is it safe to take painkillers before we get the COVID-19 vaccine? If you want to be especially careful, it is best to avoid taking over-the-counter pain medications before you get an injection. But after the COVID-19 vaccine, it’s okay to take Tylenol.
Is it safe to take aspirin while taking the COVID-19 vaccine?
â € ¢ If you are taking aspirin daily to protect your cardiovascular or cerebrovascular system, do not skip aspirin because of the COVID vaccine To see also : Indiana AG Todd Rokita says he doesn’t believe COVID-19 stats his own state releases.
How can I reduce the pain after the COVID-19 vaccine?
To reduce pain and discomfort at the vaccination site, apply a clean, cool, wet cloth to the area. Use or move your arm.
What happens if you take Tylenol before the COVID-19 vaccine?
Studies have shown that Tylenol (acetaminophen) and NSAIDs could affect the functioning of the immune system, but we do not know if this would make COVID-19 vaccines less effective. If you want to be especially careful, it is best to avoid taking over-the-counter pain medications before you get an injection.
What kind of pain reliever can you take with the COVID-19 vaccine?
Centers for Disease Control says you can take over-the-counter pain medications such as ibuprofen (such as Advil), aspirin, antihistamines, or acetaminophen (such as Tylenol) if you have side effects after being vaccinated against Covid.
Can you take Tylenol after the COVID-19 vaccine?
Experts recommend this because it can help alleviate the side effects you may experience. Read also : Are there mountain in Indiana?. Reactions you may have after vaccination are a sign that your immune system has already started to respond to the vaccine, so taking Tylenol or Advil should not affect it.
How can I reduce the pain after the COVID-19 vaccine?
To reduce pain and discomfort at the vaccination site, apply a clean, cool, wet cloth to the area. Use or move your arm.
What medications should be avoided before the COVID-19 vaccine?
It is not recommended to take over-the-counter medicines – such as ibuprofen, aspirin or acetaminophen – before vaccination to prevent vaccine-related side effects.
What is the safest medicine to take after the COVID-19 vaccine?
Helpful Hints for Relieving Side Effects Talk to your doctor about taking over-the-counter medications such as ibuprofen, acetaminophen, aspirin (only for people 18 years of age or older), or antihistamines for any pain and discomfort that occurs after vaccination.
Who are at higher risk of developing serious illness from COVID-19?
Older people and those with underlying health problems such as cardiovascular disease, diabetes, chronic respiratory disease and cancer are more likely to develop serious diseases.
Is it safe to take paracetamol before receiving the COVID-19 vaccine?
It is not recommended to take painkillers such as paracetamol before receiving COVID-19 vaccine to prevent side effects. This is because it is not known how painkillers can affect the way the vaccine works.
How long does it take for symptoms of the coronavirus disease to appear?
On average, it takes 5-6 days from the moment someone is infected with the virus for symptoms to appear, but it can take up to 14 days.
Can the Omicron variant of COVID-19 cause long-term symptoms?
Although much is still unknown about omicron, experts say this version could lead to a long-lasting Covid, even with a mild case. Patients with long-term symptoms may experience severe fatigue, irregular heartbeat, and other problems months after the first Covid infection.
Does multisystem inflammatory syndrome (MIS) often develop after recovery after COVID-19? Although very rare, some people, mostly children, experience multisystem inflammatory syndrome (MIS) during or immediately after COVID-19 infection. MIS is a condition in which various parts of the body can become inflamed.
Can COVID-19 have lasting effects?
Some people who have had severe COVID-19 disease experience inorganic effects or autoimmune conditions over time with symptoms that last for weeks or months after COVID-19 disease. Multiorganic effects can affect most, if not all, body systems, including the heart, lungs, kidneys, skin, and brain functions.
How long does the post-COVID condition last?
Although most people with COVID-19 improve in the weeks after illness, some people experience conditions after covid. COVID conditions are a wide range of new, recurring, or persistent health problems that people may experience more than four weeks after their first infection with the virus that causes COVID-19.
What are some of the common symptoms of the COVID-19 disease?
Symptoms may include: fever or chills; cough; shortness of breath; fatigue; muscle and body pain; headache; new loss of taste or smell; sore throat; stuffy nose or runny nose; nausea or vomiting; diarrhea.
How does COVID-19 affect the heart and lungs?
SARS-CoV-2, the virus that causes COVID-19, most commonly affects the lungs, but can also cause serious heart problems. Damage to the lungs caused by the virus prevents oxygen from reaching the heart muscle, which in turn damages the heart tissue and prevents it from accessing oxygen to other tissues.
What are some of the lingering side effects of COVID-19?
It’s been a whole year since the COVID-19 pandemic began, and the stunning effects of the virus continue to baffle doctors and scientists. Doctors and patients are particularly concerned about long-term side effects, such as memory loss, reduced attention span and the inability to think rationally.
What are the complications of COVID-19?
Complications may include pneumonia, acute respiratory distress syndrome (ARDS), multiorgan failure, septic shock, and death.
What are the organs most affected by COVID‐19?
The lungs are the organs most affected by COVIDâ € 19
Are smokers more likely to develop severe symptoms with COVID-19?
Current evidence suggests that the severity of COVID-19 is higher among smokers. Smoking impairs lung function, making it harder for the body to fight respiratory diseases due to the new coronavirus. Tobacco users are at higher risk of contracting the virus through their mouths while smoking cigarettes or using other tobacco products. If smokers become infected with the COVID-19 virus, they face an increased risk of severe infection, as their lung health is already at risk.
What are some of the common symptoms of the COVID-19 disease?
Symptoms may include: fever or chills; cough; shortness of breath; fatigue; muscle and body pain; headache; new loss of taste or smell; sore throat; stuffy nose or runny nose; nausea or vomiting; diarrhea.
When can COVID-19 symptoms begin to appear?
Symptoms can appear 2-14 days after someone is exposed to the virus and can include fever, chills and cough.
What are some of the most common presenting symptoms of COVID-19?
Initial presentation – Cough, myalgia and headache are the most commonly reported symptoms of COVID-19. Other characteristics, including diarrhea, sore throat, and odor or taste disturbances, are also well described (Table 3).
What are the signs and symptoms of COVID-19?
Among those who develop symptoms, most experience fever (83% -99%), cough (59-82%), fatigue (44-70%), anorexia (40-84%). ), shortness of breath (31% –40%) and myalgia (11–35%). Other nonspecific symptoms such as sore throat, stuffy nose, headache, diarrhea, nausea and vomiting have also been reported. Loss of odor (anosmia) or loss of taste (ageusia) has also been reported prior to the onset of respiratory symptoms. In particular, the elderly and patients with weakened immune systems may have atypical symptoms such as fatigue, decreased alertness, decreased mobility, diarrhea, loss of appetite, delirium, and absence of fever. Symptoms such as dyspnoea, fever, gastrointestinal symptoms (GI) or fatigue due to physiological adjustments in pregnant women, side effects of pregnancy or other diseases such as malaria may overlap with COVID-19 symptoms. Children may not report fever or cough as often as adults.
Does the COVID-19 vaccine work on new mutations?

There is promising evidence to suggest that current vaccines will protect you from most of the variants or mutations of COVID-19 currently circulating in the United States. It is possible that some variants may cause disease in some people after vaccination. However, if the vaccine proves to be less effective, it may still offer some protection. Researchers are monitoring how new versions of COVID-19 may affect how vaccines will work in real-world scenarios. To learn more about vaccines and new versions, visit the Centers for Disease Control and Prevention. (Last updated 15.6.2021)
Can Pfizer’s COVID-19 booster injection help with the Omicron version? Pfizer said this month that a booster dose of its COVID-19 vaccine could offer significant protection against a new version of omicron, although the initial two doses appear to be significantly less effective.
Should you get the Covid vaccine if you have an autoimmune disease?
The American College of Rheumatology Clinical Guidelines COVID-19 recommends that people with autoimmune and inflammatory rheumatic diseases (including lupus) receive the vaccine unless they are allergic to a component of the vaccine.
Can someone with autoimmune disease get the COVID-19 vaccine?
V. Michael Holers, head of the Department of Rheumatology at the University of Colorado School of Medicine, should have no concerns about vaccination against COVID-19 unless a person has a disappearing rare allergy to vaccine adjuvants. .
Are you at risk of experiencing an autoimmune disease flare-up from COVID-19 vaccine?
There is a risk that outbreaks may occur. In view of the above, it has been observed that people living with autoimmune and inflammatory conditions are at higher risk of severe symptoms of COVID-19 infection.
Can COVID-19 cause an autoimmune disease?
Widespread and prolonged inflammation during severe COVID-19 disease can cause the immune system to produce antibodies against pieces of the virus that it would not normally recognize. Some of these pieces could be similar enough to human proteins to trigger autoantibody production.
Do the COVID-19 vaccines protect against delta variant?
While research shows that COVID-19 vaccines are slightly less effective against the delta version, Pfizer-BioNTech, Moderna and Janssen / Johnson & Johnson COVID-19 vaccines still appear to provide protection against severe COVID-19 disease.
Is there a booster shot for the COVID-19 vaccine?
Anyone aged 16 and over can receive booster vaccination after completing the primary batch of COVID-19 vaccine. People aged 16 to 17 can receive the Pfizer-BioNTech COVID-19 booster vaccine.
Do COVID-19 vaccines protect against the delta strain?
Vaccination is the best protection against Delta. The most important thing you can do to protect yourself from the Delta is complete vaccination, doctors say.
Does the COVID-19 vaccine help against different strains?
Do vaccines work against new strains? A simple answer is yes. There is currently no evidence to suggest that these or any other variants of COVID-19 are resistant to current vaccines.
Should I wear a face mask even if I am vaccinated against COVID-19?
Yes, vaccinated people must continue to wear a face mask when visiting enclosed public spaces or using public transportation in areas where COVID-19 is transmitted in the community. The vaccine is very effective in preventing serious illness and death, but vaccinated people can still become infected and transmit the infection. Wearing a face mask reduces the risk of this.
What are the organs most affected by COVID‐19?
The lungs are the organs most affected by COVIDâ € 19
Can COVID-19 spread through water while swimming?
Fact: Water or swimming does not transmit the COVID-19 virus. The COVID-19 virus is not transmitted through water during swimming. However, the virus spreads among people when someone has close contact with an infected person. WHAT YOU CAN DO: Avoid crowds and maintain a distance of at least 1 meter from others, even when swimming or swimming. Wear a mask when you are not in the water and cannot stay away. Wash your hands often, cover your cough or sneeze with a handkerchief or bent elbow, and stay home if you don’t feel well.
Is the Mu variant of COVID-19 a ‘variant of interest’?
Although the World Health Organization continues to rank Mu as a “version of interest” around the world, the CDC cites Mu simply as a “version that accompanies it”. ‘The CDC counts 10 variants in the group of variants being monitored, including three that were once considered variants: alpha, beta and gamma
When was the Mu COVID-19 version first discovered? The epicenter of its transfer is Colombia, where the variant was first isolated on 11 January 2021 (Figure 1A and Table S2). From March to July 2021, the number of Covid-19 cases in Colombia increased sharply.
Are new variants of COVID-19 possible?
New versions of the virus are expected to emerge. Measures to reduce the spread of infection, including the COVID-19 vaccine, are the best way to slow the emergence of new variants.
Is it possible to get the same strain of COVID-19 twice?
Re-infections with COVID-19 are rare, but they do occur. Re-infections could become more common over time and as new versions of COVID-19 emerge.
Are some COVID-19 variants more dangerous?
Some versions seem to spread easier and faster than other versions, which may result in more COVID-19 cases. An increase in the number of cases will increase the burden on health resources, lead to more hospitalizations and potentially more deaths.
How do new variants of COVID-19 occur?
Viruses are constantly changing with mutations and sometimes these mutations cause a new version of the virus. Some versions appear and disappear, while others persist. New versions will continue to appear.
What is the difference between a variant and a lineage for COVID-19?
Viruses such as SARS-CoV-2 are constantly evolving as defects (gene mutations) occur during genome replication. The line is a genetically closely related group of virus variants derived from a common ancestor. The variant has one or more mutations that distinguish it from other variants of the SARS-CoV-2 virus.
What is the difference between the original COVID-19 virus and the Delta variant?
The Delta version causes more infections and spreads faster than the original strain of SARS-CoV-2 virus, which causes COVID-19. Vaccines remain the best way to reduce the risk of serious illness, hospitalization and death from COVID-19.
How do new variants of COVID-19 occur?
Viruses are constantly changing with mutations and sometimes these mutations cause a new version of the virus. Some versions appear and disappear, while others persist. New versions will continue to appear.
Does the COVID-19 Delta variant cause more serious illness?
â € ¢ Some data suggest that the Delta variant could cause more serious diseases than previous strains in unvaccinated individuals. In two different studies from Canada and Scotland, patients infected with the Delta variant were more likely to be hospitalized than patients infected with alpha or original virus strains.
What is a COVID-19 variant of interest?
A variant with specific genetic markers associated with changes in receptor binding, decreased neutralization with antibodies generated against previous infection or vaccination, reduced treatment efficacy, potential diagnostic effects, or predicted increases in disease transmission or severity.
Is the COVID-19 Epsilon variant more infectious?
The Epsilon version is becoming increasingly recognizable as the number of COVID-19 cases among the unvaccinated has increased, in part due to the expanded Delta version. In the lab, the Epsilon version proved to be more contagious than previous versions, and researchers found three changes in its protein tips.
What is the difference between the original COVID-19 virus and the Delta variant?
The Delta version causes more infections and spreads faster than the original strain of SARS-CoV-2 virus, which causes COVID-19. Vaccines remain the best way to reduce the risk of serious illness, hospitalization and death from COVID-19.





Comments are closed.